“Mindfulness isn’t difficult, we just need to remember to do it.” — Sharon Salzberg
The ability to walk is something many of us, myself included, have always taken for granted. Now that I have Parkinson’s disease (PD), something that used to come as a matter of course to me is starting to deteriorate. PD has adversely affected my left side more than my right side. I find myself tripping more, since I tend to drag my left foot.
Walking now requires my conscious thought
Going for a walk is now more of a mindful task than an exercise for me. I find it much more therapeutic to focus on how I walk and be in the present moment than to think about the future and how my PD may progress. With each step I take, I concentrate on repeating to myself, “Heel, toe.”
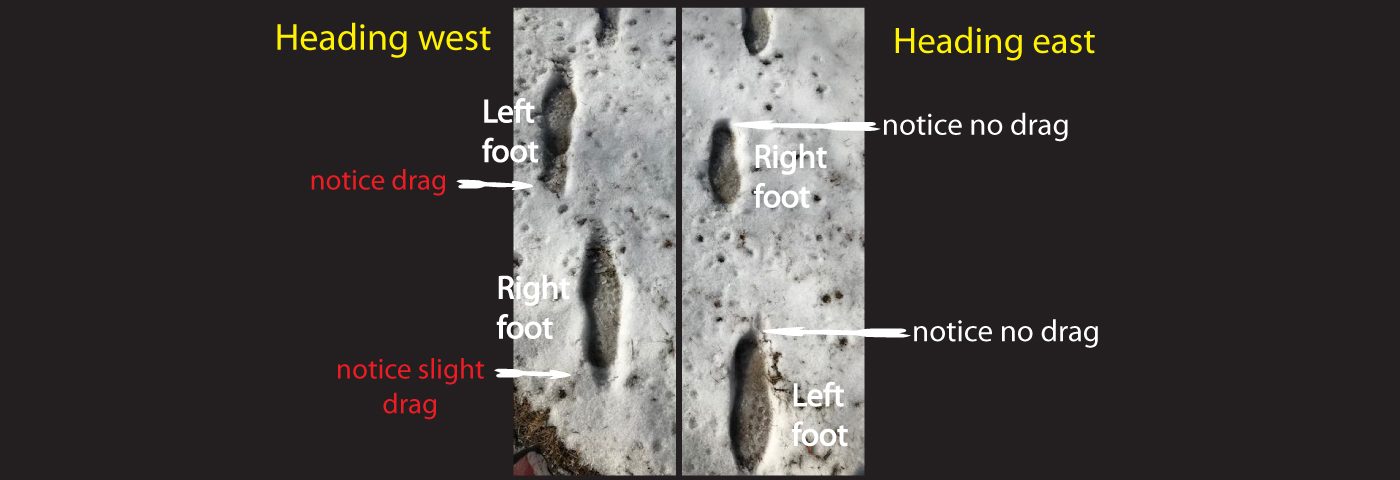
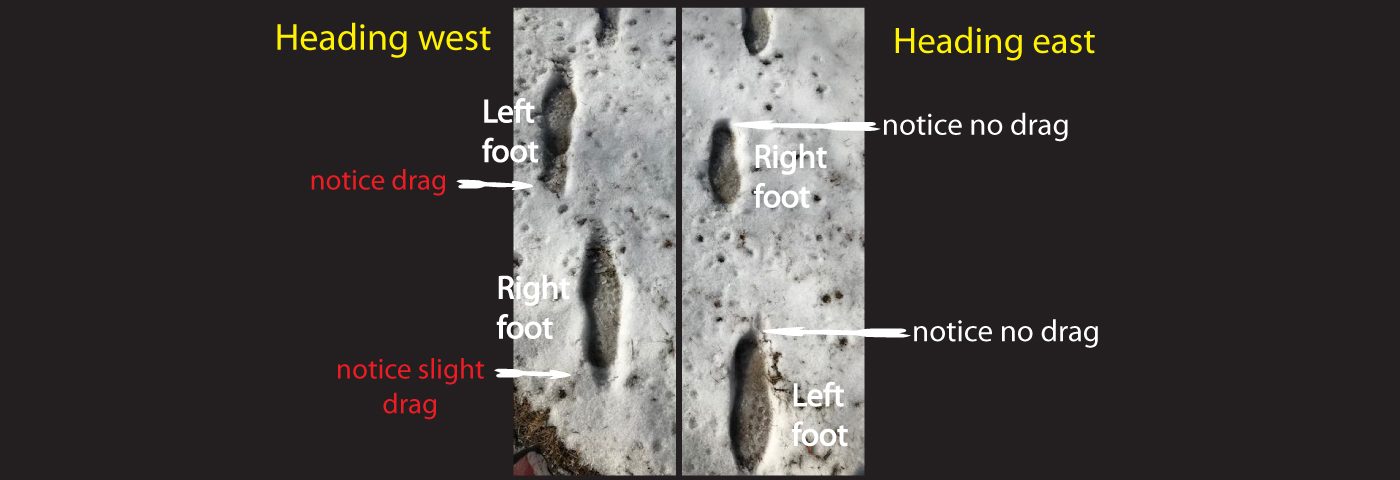
When there was snow on the ground, I decided to compare my walking steps when I did not focus on saying “heel, toe” with those from when I did. My footprints in the snow were very telling, so I took a photograph. On the left side of the photo are my steps when I was not thinking about my stepping patterns. You might notice that both feet show a bit of a drag in the snow. On the right side of the photo, as I moved forward, I really focused on flexing both of my feet and having my heel strike first. There are no signs of drag on either foot.
Am I putting too much thought into this?
Years of training to improve as a dancer and a cyclist have made analysis of my body movements come quite naturally to me. Whether it was improving my pedal stroke for more cycling power or perfecting my balance to do pirouette turns, I learned to be mindful and to be in touch with how my body was performing. Now I must use that skill to help myself be more attentive when I walk.
My neurologist says I tend to overthink things. I believe our greatest strengths can also be our greatest weaknesses. Sometimes, I do overthink, to the point of getting paralysis by analysis. However, I believe that mindful analysis of my PD symptoms (including my walking technique) is critical in helping me to create different ways of doing things that at one time (before PD) used to come as second nature to me.
Recent Comments